AMD / Macular Degeneration
Age-related macular degeneration (AMD) is a common disease of the retina. The macula is the central, most important area of the retina. A normal macula provides the detailed vision required for reading and distance vision. Changes in the macula due to age can cause a decrease in how well the macula works. In most cases, these changes occur gradually over many years.
In early stages, AMD causes no symptoms. As the disease progresses, it may cause blurry vision or difficulty with reading vision. In advanced cases, AMD can cause a devastating loss of central vision, limiting a person’s ability to even recognize someone’s facial features. It is the number one cause of legal blindness in Americans over the age of 60. It does cause total blindness as only the central part of the retina is affected. Peripheral or side vision is unaffected by macular degeneration.
What types of Macular Degeneration are there?
There are two forms of AMD – Dry and Wet. About 90% of people who have AMD have the dry form of the disease. This can be very mild and may not cause any changes in vision at all. Some people with the dry form will go on to develop changes in the pigmented tissue underneath the macula. This may cause a gradual decrease in central vision.
About 10% of people with AMD develop the wet form of the disease. This occurs when abnormal blood vessels (choroidal neovascularization) develop underneath the macula. These blood vessels leak fluid and blood and eventually cause scarring of the macula. Dry AMD may progress to wet AMD, without warning, at any time.
Who is at risk?
AMD affects people over the age of 55. The risk of developing AMD increases with age. Approximately 28% of people over the age of 75 have some form of AMD. Although we do not know exactly why AMD develops, we do know that it tends to run in families. Risk factors for AMD include high blood pressure, obesity, ultraviolet light exposure and smoking. Studies have shown that smoking greatly increases the risk of developing advanced AMD.
What are the symptoms?
The early stages of dry AMD cause little to no visual symptoms for most people. Some will notice a gradual decrease in reading vision. It is also common to have some fluctuating vision, especially after being exposed to a bright light or sunlight.
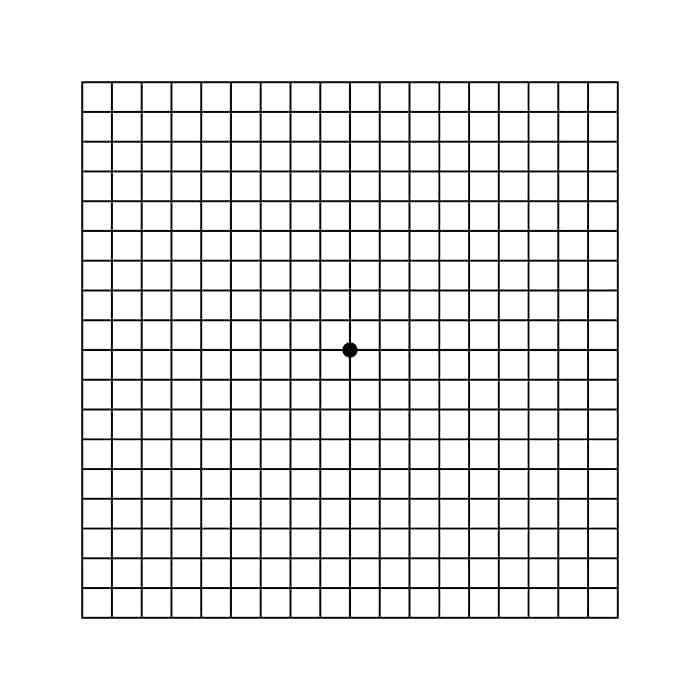
Wet AMD can cause a sudden loss of central vision. Patients will often notice that objects become distorted, straight lines appear wavy, and some will describe a blind spot in their central vision. Some people are unaware of changes in vision due to wet AMD as it tends to affect only one eye at a time.
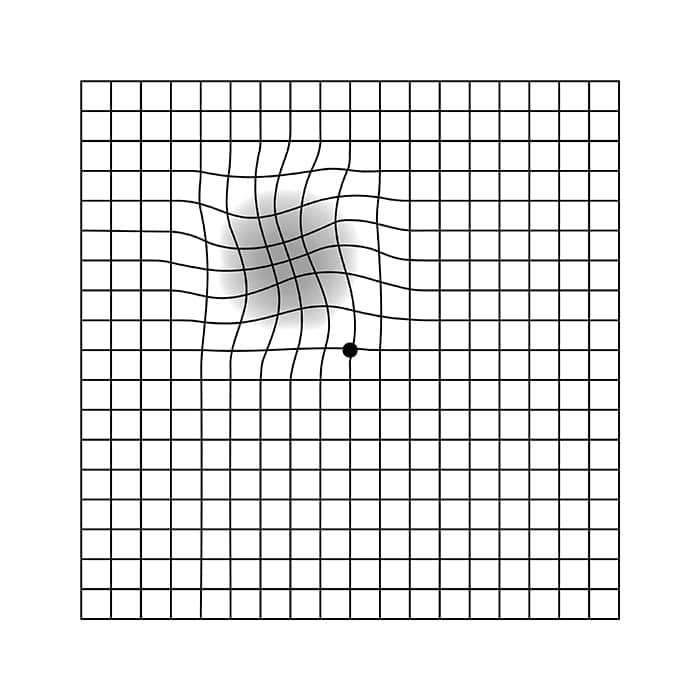
One of the best ways for anyone with AMD to monitor their vision is with a simple test called the Amsler grid. Any sudden grid changes should be reported to your doctor immediately.
What will my doctor see?
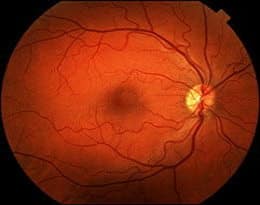
AMD can only be diagnosed by an eye care professional, generally through a dilated eye examination. The outside of the eye appears completely normal.The earliest sign of AMD is the presence of small yellow deposits in the macula called drusen. Changes to the pigmented tissues in the macula develop as the disease progresses. Macular pigment can wither away in a process called atrophy. Atrophy causes a more significant loss of central vision. Drusen formation, pigment changes, and atrophy are all due to dry AMD.
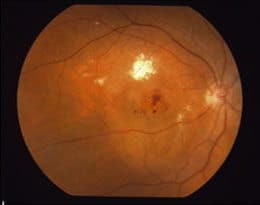
Fluorescein angiography, a test using an intravenous dye and photography to analyze retinal blood vessels, is often used to diagnose wet AMD. The results of this test help determine treatment options for patients with wet AMD.
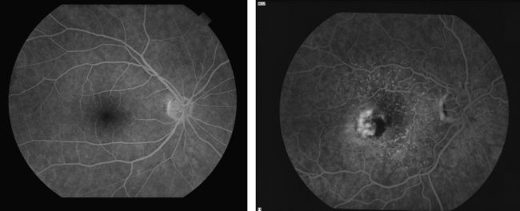
LEFT: Fluorescein angiography showing a normal macula
RIGHT: Fluorescein angiography showing wet AMD
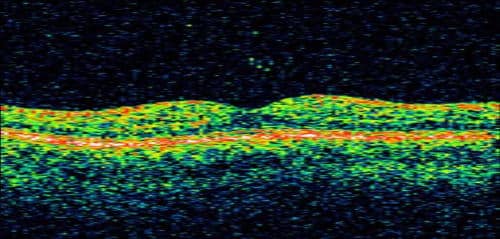
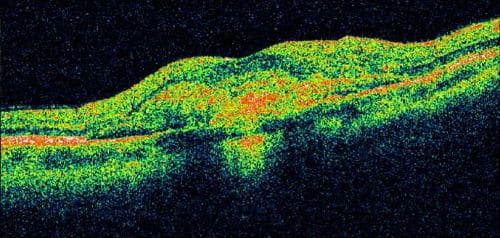
Optical Coherence Tomography(OCT)is also an important test in assessing AMD, both in diagnosis and response to treatment. OCT can reveal microscopic changes in the architecture of the macula, including retinal swelling, fluid and atrophy that often cannot be detected during a clinical exam.
What treatments are currently available?
There is no known cure for macular degeneration. The goal of any treatment is to preserve vision. Treatment is generally recommended if patients develop wet AMD. Treatment options include:
Traditional focal laser:
In this type of treatment, a laser is applied to the abnormal vessels near, but not directly in, the central macula. A small blind spot will occur as a result of this treatment. Most patients with wet AMD are not good candidates for this treatment as abnormal blood vessels tend to grow in the very center of the macula.
Photodynamic therapy (PDT):
Introduced in 2000, this treatment has been shown to slow the rate of vision loss associated with abnormal blood vessel growth underneath the central macula. A special light-sensitive medication (Visudyne™) is injected into the arm and the dye is activated in the macula by a special “cold” laser. This technique allows treatment of abnormal blood vessels without causing significant damage to the surrounding retinal tissue. This treatment often needs to be repeated every 3 months over the span of 1 to 2 years. The medication can be activated in other parts of the body by sunlight, and great care must be taken to avoid the sun or any bright light for several days following the procedure. Currently, this treatment is not used often.
Vascular Endothelial Growth Factor (VEGF) Inhibitors:
Most patients with active wet AMD benefit from treatment with VEGF inhibitors. These medications block the effects of a specific protein growth in the eye that causes abnormal blood vessel development. Injections of the medication directly into the eye can be done safely in an office setting.
- Lucentis®: Lucentis is a powerful agent that block all active forms of VEGF in the eye. This is the first treatment for wet AMD that was able to show long-term vision improvement in patients involved in large clinical trials.
- Avastin®: Avastin and Lucentis are closely related medications. In fact, they were developed by the same company. Avastin is approved for treatment of certain types of cancer, and has not been approved specifically for use in the eye. However, Avastin is routinely used throughout the United States in patients with wet AMD, primarily due to cost. While the effects of the medications appear to be similar, Avastin treatment for wet AMD is much less expensive than Lucentis.
- Eylea®: This is the newest medication approved for use in wet AMD. It acts in a slightly different manner than Lucentis and Avastin and may be more effective in certain cases.
Can Macular Degeneration be prevented?
People who are at risk for developing AMD should have a dilated eye exam once a year. Early changes indicating macular degeneration can often be detected by eye care professionals before any symptoms occur.
Smoking is the most significant controllable risk factor for macular degeneration. Anyone with macular degeneration or a family history of macular degeneration should definitely not smoke. Eating healthy, controlling blood pressure, exercising regularly, and wearing sunglasses that filter UV light all likely decrease the risk of developing macular degeneration.
Vitamin supplements for the eye, specifically anti-oxidants (Beta-carotene, vitamins C and E) and zinc, have been shown in a large clinical study to be effective at slowing macular degeneration progression. Patients who have early to moderate AMD should be taking an over-the-counter vitamin supplement such as Ocuvite Preservision, Icaps, or Viteyes. Only an eye care professional can determine if someone is likely to benefit from this type of supplement. Smokers or former smokers should take a supplement without beta-carotene, as this can increase the risk of lung cancer in these individuals.
There is a large clincal trial investigating the relationship between Omega-3 fatty acids (fish oil, etc.) and AMD. Some small studies have shown a decrease in AMD progression with this type of supplement. Lutein, found in spinach, kale and in vitamin supplements, has also been shown to slow AMD.
Millions of dollars each year are spent investigating better ways to treat, and perhaps eventually cure, AMD. Clinical trials investigating treatment of both dry and wet AMD are ongoing.